24 Apr. 2019. Researchers at Arizona State University created a process to make the genome editing technique Crispr less likely to cause an immune system reaction in patients. A team from the university’s Biodesign Institute in Tempe explains the process in yesterday’s issue of the journal Nature Communications.
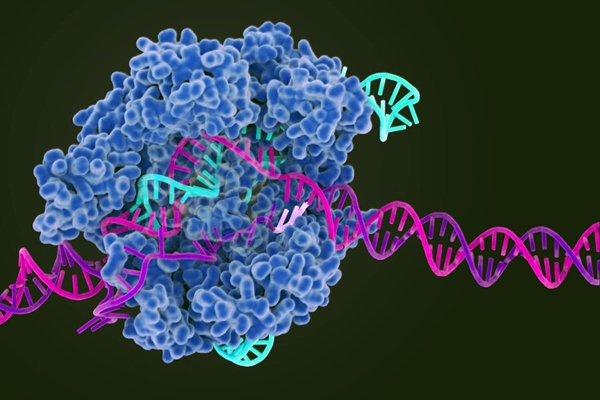
Since its initial publications in 2012, Crispr — short for clustered, regularly interspaced short palindromic repeats — makes it possible to edit genomes of organisms by harnessing bacterial defense mechanisms that use RNA to identify and monitor precise locations in DNA. Bacteria defend themselves against viruses by taking pieces of the invading viral DNA into their cells to protect themselves against further attacks. That protection is provided by ribonucleic acid or RNA expressed by the DNA pieces taken before to find the same sequence of genes in the invaders’ DNA. At that point, an enzyme cuts the DNA at the designated spot, killing the virus.
That enzyme is called Crispr-associated endonuclease 9, or Cas9, which is the leading enzyme for editing DNA studied with Crispr and in use today. In most of today’s Crispr systems, RNA guides Cas9 enzymes to the targeted gene sequence, where Cas9 performs the editing, making it possible in gene therapies to address root causes of some diseases by removing or changing specific genes.
While Crispr may make it easier to edit gene sequences, it isn’t foolproof. Samira Kiani, a biomedical engineering professor at the Biodesign Institute and co-leader of the project, notes in a university statement, that scientists need to account for “ethical, societal, safety, and regulatory considerations related to Crispr usage. Safety engineering to address controllability, specificity, and side effects of Crispr treatments have gained significant momentum and ethical debates have arisen to ensure correct use of technology.”
Among the safety concerns with Crispr in gene therapies is adverse effects caused by the Cas9 enzyme. Cas9 is derived from streptococcus pyogenes bacteria, the same common bacteria responsible for strep throat, scarlet fever, impetigo, and other diseases. And people with those diseases develop antibodies in their immune systems that react when in the presence of anything resembling streptococcus pyogenes, such as Cas9. “The problem,” says Karen Anderson, the project co-leader and Arizona State medical school professor, “is that many of us are already immune to streptococcus. If you have had a Group A strep infection, you may have preexisting immunity to that protein.”
The Arizona State team tested the blood of 143 healthy volunteers and found 82 in the group, or 57 percent, with antibodies to streptococcus pyogenes, which highlights the potential difficulty with Cas9 enzymes in Crispr-based therapies. To meet this challenge, the researchers genetically engineered the gene expressing the Cas9 enzyme to deactivate the chemical binding sites, called epitopes, used by antibodies, while still taking care to preserve Cas9’s DNA cutting ability. In lab tests using blood samples with antibodies to streptococcus pyogenes, the altered Cas9 does not invoke reactions in immune system cells. And further tests show the engineered Cas9 retains its DNA editing functions.
“We took those dominant epitopes and tried to silence them”, adds Anderson, “just by doing one or two mutations in the Cas9 gene. “But we rebuilt it, so the gene was still functional. It’s not immunologically silent, but its more quiet.” The university applied for a patent on the technology’s use in gene therapies.
More from Science & Enterprise:
- Trials Underway Testing Crispr for Blood Disorders
- Infographic – What is Crispr?
- Trials OK’d for Inherited Eye Disease Therapy with Crispr
- Allergan Licensing Crispr for Inherited Eye Disease
- More Damage Detected from Crispr-Cas9 Edits
* * *

 RSS - Posts
RSS - Posts
[…] Crispr Made More Immune-System Safe […]