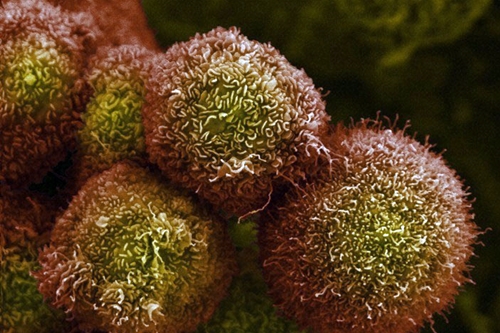
Pancreatic cancer cells in culture (Anne Weston, London Research Institute, via National Institute of General Medical Sciences)
Updated 4 October 2016. A large-scale clinical trial is planned to test treatments for pancreatic cancer guided by the genomics of a patient’s own tumor. The trial, called Precision Promise, will be conducted at 12 sites in the U.S. by a consortium led by Pancreatic Cancer Action Network, committing $35 million to the project over 4 years.
Pancreatic cancer is often difficult to diagnose in its early stages, because of few unique symptoms associated with the disease, and because the pancreas is hidden among other organs in the body. As a result, it is often diagnosed in later, more advanced stages of the disease, with generally a poor prognosis for survival: 5-year survival rate of only 8 percent. American Cancer Society estimates more than 53,000 people in the U.S. will be diagnosed with pancreatic cancer this year, leading to nearly 42,000 deaths.
Pancreatic Cancer Action Network says one difficulty finding treatments for this type of cancer is the low rate of participation in clinical trials by patients, about 4 percent. The organization hopes the approach of Precision Promise will make treatments more customized and work faster than traditional clinical trials, thus attracting more participants. In an organization statement, president and CEO Julie Fleshman says, “Instead of looking for the right patient for a clinical trial, we are designing the right clinical trial for each patient.”
Precision Promise initially plans 3 different therapy approaches, based on the state and composition of the patients’ tumors. “We will be able to offer options to patients based on the molecular profile of their tumor,” says Victoria Manax Rutson, chief medical officer of Pancreatic Cancer Action Network, “rather than trying to fit them into a clinical trial that may not suit the needs of their disease.” The organization expects to recruit “thousands” of patients in the study, although enrollment targets were not disclosed.
When the trial begins in the spring of 2017, patients will first have their tumors analyzed at one of the 12 medical center sites, and then assigned to one of the 3 sub-studies testing therapy strategies that best matches their molecular profile:
– Repair of damaged DNA
– Disruption of stroma, tumor support structures
– Immunotherapy
The study may add sub-studies for other treatment options if supported by evidence from patients. Participants in the trial can also change from one sub-study to another, if their tumors evolve and other therapies become more appropriate.
The 12 medical center sites for Precision Promise are Cedars-Sinai in Los Angeles, Dana-Farber Cancer Institute in Boston, Fred Hutchinson Cancer Research Center in Seattle, Memorial Sloan Kettering Cancer Center in New York, University of California in San Diego, University of California in San Francisco, University of Chicago, University of Florida in Gainesville, University of Michigan in Ann Arbor, University of Pennsylvania in Philadelphia, Virginia Mason in Seattle, and Washington University in St. Louis.
Pancreatic Cancer Action Network is partnering with health technology company Tempus in Chicago, which will provide genomic sequencing services for Precision Promise. The company expects to apply its machine learning and algorithms to the massive amounts of data generated by the analyses. Cancer Research And Biostatistics, a not-for-profit organization in Seattle, will provide further statistical analysis and data management.
Update, 4 October 2016. Two more enterprises are taking part in Precision Promise. Halozyme Therapeutics, a biotechnology company in San Diego, is providing its experimental drug code-named PEGPH20, a synthetic enzyme that degrades hyaluronan in human tissues. Hyaluronan is a naturally occurring gel-like substance found in skin and cartilage, but also the microenvironment supporting tumor cells.
In addition, Trovogene Inc., also in San Diego, is providing its liquid biopsy technology making it possible for closer tracking and evaluation of treatments. Trovogene’s technology detects and monitors circulating tumor DNA in blood and urine, reducing the need to take tissue-sample biopsies that require surgery.
Read more:
- Genentech, BioNTech Partner on Personal Cancer Therapies
- St. Jude, Sanger Institute to Share Genomic Databases
- Amgen, Advaxis Partner on Personal Cancer Immunotherapy
- Moderna, Merck Partner on Personal Cancer Vaccines
- Precision Medicine Shown to Boost Cancer Outcomes
* * *

 RSS - Posts
RSS - Posts
[…] Precision Medicine Trial Set for Pancreatic Cancer […]