9 October 2014. Researchers at Harvard University developed a technique that enables embryonic stem cells to transform into large quantities of insulin-producing beta cells found in the pancreas, a key step in developing a treatment for type 1 diabetes. The team led by biologist Douglas Melton, co-director of the university’s Stem Cell Institute, published its findings today in the journal Cell (paid subscription required).
Beta cells in the pancreas, when functioning properly, produce insulin, a hormone that helps the body store and process glucose provided by food in the diet. People with type 1 diabetes, a condition where the body’s immune system is tricked into destroying beta cells. Some 3 million people in the U.S. have type 1 diabetes, including many children and young adults, who need to replace their insulin supply daily through injections or devices such as insulin pumps.
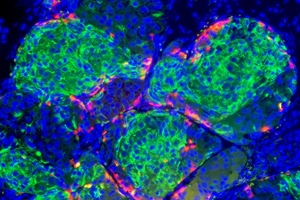
Melton and colleagues designed a culturing protocol for transforming human embryonic stem cells into pancreatic and endocrine progenitor cells, and then into beta cells. Their techniques enabled the team to generate hundreds of millions of beta cells in the lab that perform the same insulin-secreting functions, responding to glucose as normal mature beta cells. Tests of the beta cells show their genes express similarly to normal beta cells.
The researchers then implanted the lab-produced beta cells in mice where the cells secreted insulin in response to glucose as they had done in lab cultures. In addition, the team induced a diabetic state in lab mice, and found transplants of the lab-produced beta cells relieved hyperglycemia, a high blood glucose condition, in the test mice. Harvard says Melton’s lab is also testing stem-cell derived beta cells in monkeys.
For Melton, the issue of type 1 diabetes is personal. The university says his son and daughter were diagnosed with the disorder as children, and he made finding a cure the goal of his career. Melton is collaborating as well with MIT biomedical engineer Daniel Anderson to develop a device that protects the 150 million implanted beta cells from immune-system attack. Preclinical tests of the device with lab mice indicate the device can protect the cells for months while they continue to produce insulin.
Read more:
- Investment Fund Launches to Support Stem Cell Ventures
- Advance Achieved in Replacement Kidney Blood Vessels
- Chip Device Developed to Quickly Test for Type 1 Diabetes
- Quality Assurance Techniques Proposed for Stem Cells
- Calif Stem Cell, UC Irvine Partner on Eye Transplant Tissue
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.