2 September 2015. A large-scale study of preexposure prophylaxis or PrEP, the use of antiviral drugs to prevent HIV infection, found the practice prevented new HIV infections among Kaiser Permanente clients in San Francisco over a 32-month period. Results of the study led by Kaiser Permanente epidemiologist Jonathan Volk, appear in yesterday’s issue of the journal Clinical Infectious Diseases (paid subscription required).
Kaiser Permanente is a California-based health care plan and provider that includes a research division conducting epidemiological and health services studies. In 2012, the U.S. Food and Drug Administration approved the combination of anti-viral drugs emtricitabine and tenofovir to prevent HIV among people at high risk of infections. Volk and colleagues looked into the efficacy of PrEP in a long-term, real world setting, which they say is so far evaluated only in clinical trials and demonstration projects.
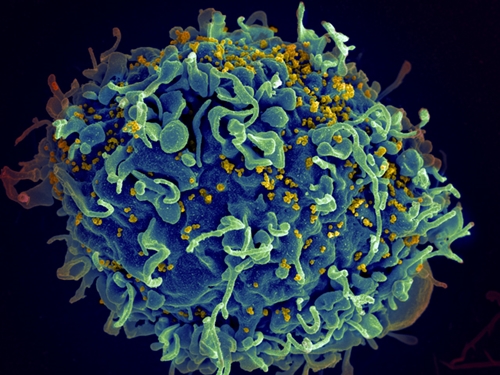
The drugs emtricitabine and tenofovir are administered as a single pill taken daily, marketed as Truvada by Gilead Sciences. Truvada is a type of drug known as nucleoside reverse transcriptase inhibitors that works by blocking an reverse transcriptase enzyme.
Blocking the enzyme prevents the HIV virus from multiplying, and causes the amount of HIV in the body to decline. The drug is given along with advice to perform safe sex to reduce HIV infections in adults, even after infections are diagnosed, and is also approved by FDA to treat HIV infections.
The Kaiser Permanente team tracked referrals to its San Francisco medical center over a 32-month period. During that time, the center received 1,045 referrals for PrEP, of which 657 individuals began the regimen. Virtually all (99%) of the individuals were men having sex with other men, and averaged 37 years of age. People receiving PrEP medications were more likely to have multiple sex partners than individuals not taking PrEP drugs, but less likely to have a partner with HIV.
During the observation period, no new HIV infections were reported among PrEP participants, but sizable percentages of other sexually transmitted infections were reported. After 6 months, some 30 percent of PrEP participants reported at least one sexually transmitted infection, with that percentage rising to half (50%) after 12 months. Chlamydia, rectal infections, and gonorrhea were those reported most often.
Among people receiving PrEP, the length of time taking the drugs was about 7 months, but they report a mixed record of sexual behavioral change. After 6 months of use, about three-quarters (74%) of people receiving PrEP said their number of sexual partners did not change, while 15 percent said the number of partners decreased and 11 percent said the number of partners increased. Condom use, however, decreased among 41 percent of PrEP participants, while increasing among only 3 percent, and 56 percent going unchanged.
The authors recommend ongoing screening for sexually-transmitted infections, such as hepatitis C, as well as outreach to PrEP candidates other than gay men, including injected drug users, transgender women, and heterosexual men and women.
Read more:
- FDA Approves Pediatric HIV Drug Formulation
- GSK, UNC Chapel Hill Partner on HIV/AIDS Cure
- Early Trial Shows Gene Editing Potential to Treat HIV/AIDS
- Community Pharmacies Found Helpful in Encouraging HIV Tests
- Algorithm Identifies HIV Antibodies For Vaccine Design
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.