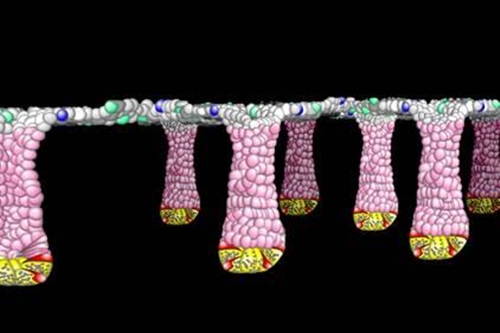
Schematic illustration of colon tissue with pits inhabited by stem cells at the bottom, and precursor and differentiated cells rising to the top. (Scott Magness, University of North Carolina, Chapel Hill)
9 October 2015. A team of medical researchers and engineers in North Carolina is developing a miniaturized device derived from human stem cells to better simulate the workings of a human gut. The five-year project is funded by $5.3 million grant from National Institute of Diabetes and Digestive and Kidney Diseases, part of National Institutes of Health.
The North Carolina team aims to design a device that more accurately reflects the workings of complex human intestinal functions, which if successful can provide more reliable simulations than tests with lab animals or simple microfluidic labs-on-chips. A better test device can improve discovery and testing of drugs for potential toxic effects on humans earlier in the development process that can translate into considerable savings from avoiding failed expensive clinical trials.
The research team is led by Nancy Allbritton who chairs a biomedical engineering department with faculty from both North Carolina State University in Raleigh and University of North Carolina at Chapel Hill, and the research team draws from both campuses. The researchers plan to design and test a working three-dimensional miniaturized replica of the human intestine that reflects its complex functions.
A key difference between the simulacra, as they call it, and earlier attempts to develop a gut-on-a-chip will be use of stem cells from human colon surfaces, arrayed on hydrogel scaffolding or framework. These stem cells will be derived from biopsies, or tissue samples from humans, and cultured to grow into intestinal tissue cells and stem cells that inhabit pits or crypts in the gut. These tissue cells will grow on hydrogel designed to absorb water and provide the biochemical stimuli to support intestinal tissue growth.
This hydrogel then will provide the environment to simulate human intestinal functions, as well as support microbes, estimated to number in the trillions that affect a wide range of biological activities in humans. These communities of microbes help process chemicals in drugs and toxins they may generate, as well as influence the release of hormones making an impact on human behavior.
Among the project’s objectives is to apply these concepts to developing personalized simulacra reflecting conditions in guts of individual patients. A personalized gut model would make it possible, say the researchers, to observe human intestines as they transform from healthy to disease states, and better track causes and effects of those transformations.
The research team plans to build on proof-of-concept work in Allbritton’s lab developing a prototype derived with cells from lab mice. One of the co-investigators, Chapel Hill medical professor Scott Magness, has been banking tissue samples for several years from routine colonoscopies at university hospitals in anticipation of this project.
Read more:
- Partnership to Study Biomarkers in Liquid Biopsies
- Lab-On-Chip Device Captures Circulating Tumor Cells
- Small Business Grant Funds Point-of-Care Sickle Cell Test
- Synthetic Platelet-Like Particles Developed, Tested
- Biochemical Signaling Chip Design Techniques Devised
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.