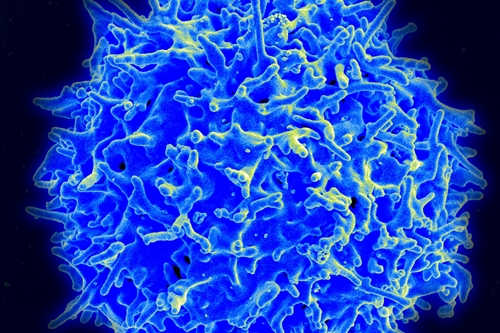
Scanning electron micrograph of a human T-cell lymphocyte (National Institute of Allergy and Infectious Diseases, NIH)
1 March 2017. A clinical trial testing synthetic immune system cells shows after 6 months the cells can generate a full or partial response in many patients with non-Hodgkin lymphoma. The trial, testing a therapy for blood-related cancers known as axicabtagene ciloleucel made by Kite Pharma, also reported a continuing problem of high adverse event rates among participants.
Kite Pharma, in Santa Monica, California, develops personalized treatments for cancer with synthetic T-cells from the patient’s own immune system. The treatments in this case address non-Hodgkin lymphoma, a cancer of lymph tissue that forms part of the body’s immune system. There are different types of non-Hodgkin lymphoma reflecting different types of white blood cells. Most adults with the disorder have either diffuse large B-cell lymphoma, which is usually aggressive, and follicular lymphoma, a slower growing cancer.
Axicabtagene ciloleucel takes T-cells from the patient, then genetically engineers the cells to produce chimeric antigen receptors on the cell surface that attract an antigen — a protein generating antibodies — fighting the cancer. The engineered T-cells are then grown in the lab in large quantities and infused back into the patient, where they attract the antigen proteins and fight the cancer. Early clinical trials of this technique, known as CAR-T says National Cancer Institute, show the technique has promise against advanced blood-related cancers, such as non-Hodgkin lymphoma.
Kite Pharma yesterday reported results from a 6-month follow-up review of participants in an early- and intermediate-stage clinical trial testing the treatment’s safety and efficacy in patients with aggressive cases of diffuse large B-cell lymphoma (DLBCL), transformed follicular lymphoma (TFL), and primary mediastinal large B-cell lymphoma (PMBCL), a rare form of the disease. The study tested for complete or partial response to the treatments with standard diagnostic definitions following the treatments and over one year, as well as watching for adverse reactions.
Of the 101 participants in the trial, 36 percent achieved a complete response from the treatments after 6 months, while another 5 percent showed a partial response. Those percentages are down from response rates reported immediately after the treatments, where more than half (54%) showed a complete response and 28 percent a partial response. Response rates were somewhat higher for TFL or PMBCL forms of the disease, where half of the group reported a complete response after 6 months.
Among patients with DLBCL, the most common form of the disease, 31 percent after 6 months were shown with a complete response. In addition, Kite Pharma says to date, the median overall survival time of patients in the trial, standing at 8.7 months, has not yet been reached.
As noted by Science & Enterprise in September 2016, many participants in this trial had serious adverse effects from the treatments after 3 months, and that pattern continued in the 6-month follow-up. Between 20 and 43 percent of participants reported side effects at least severe enough to require hospitalization from anemia, low white blood counts, low platelet counts, encephalopathy or altered brain functions, and lower lymphocyte counts.
Compared to the 3-month report, says Kite Pharma, rates of severe cytokine release syndrome and related neurological events decreased. Cytokine release syndrome occurs when enzymes are emitted from cells targeted by treatments, causing flu-like symptoms such as fevers, nausea, and muscle pain, but also neurological symptoms including hallucinations and delirium.
In our September story, we reported on 2 deaths among participants in the trial related to the treatments from hemophagocytic lymphohistiocytosis, a rare life-threatening disorder from overactive immune system cells, and cardiac arrest. The company says a third death occurred among participants, from a pulmonary embolism or blood clot in the lungs, which was unrelated to the treatments.
Axicabtagene ciloleucel received a breakthrough therapy designation in December 2015 from Food and Drug Administration for the three types of non-Hodgkins lymphoma in the clinical trial. FDA grants a breakthrough designation for new therapies to treat serious or life-threatening conditions that demonstrate substantial improvements over current treatments. Kite Pharma plans to provide full results from the trial in April at a meeting of the American Association for Cancer Research.
More from Science & Enterprise:
- Safer Engineered-Cell Cancer Immunotherapy Designed
- Brain Cancer Regression Shown with Engineered T-Cells
- Engineered T-Cells Tested on Metastatic Cancer
- High Leukemia Remissions Reported for Engineered T-Cells
- Engineered T-Cell Trial Halted After Participant Dies
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.