21 Nov. 2018. An engineering lab develop a new hydrogel with readily available materials that in lab tests promotes healing of wounds similar to those encountered by people with diabetes. Results of the research by a team from University of New Hampshire in Durham appear in this week’s print issue of the journal ACS Applied Bio Materials (paid subscription required).
The New Hampshire chemical engineering lab led by Kyung Jae Jeong studies engineered materials applied to biomedical needs, including tissue wounds and vision problems that results from diabetes, a growing public health problem in the U.S. People with diabetes often develop slow-healing skin ulcers on their feet, a common complication of the disease. In diabetes, blood flow is reduced to the legs and feet, leading to nerve damage and reduced feeling in those regions, as well as slower healing of wounds. Centers for Disease Control and Prevention says in 2010, some 73,000 Americans required amputation of a leg or foot because of complications from diabetes.
In addition, high levels of blood sugar can cause serious complications in people with diabetes, including vision problems. Among these issues is damage to the fine blood vessels in the retina, located in the back of the eye that detects and converts light to signals sent through the optic nerve to the brain. Diabetic retinopathy is the name given to this condition that can range from mild leakage in the eye to swelling and distortion of the blood vessels, and proliferation of new blood vessels to compensate for the damage.
Jeong and colleagues work with hydrogels, water-based polymers that form into gels, as vehicles for wound healing, but in most forms today are not often useful. “While valuable for helping patients,” says Jeong in a university statement, “current hydrogels have limited clinical efficacy. We discovered a simple solution to make the hydrogels more porous and therefore help to speed up the healing.”
The pores in most hydrogels are too small to allow cells to flow through and help repair the wounds. The researchers devised a process for making a hydrogel with larger pores to allow for easier cell transport. Their method involves the enzyme transglutaminase derived from microbes. Transglutaminase promotes the formation of peptide bonds, short chains of amino acids, between proteins, is often used in baking and to make edible films, and is also inexpensive and readily available.
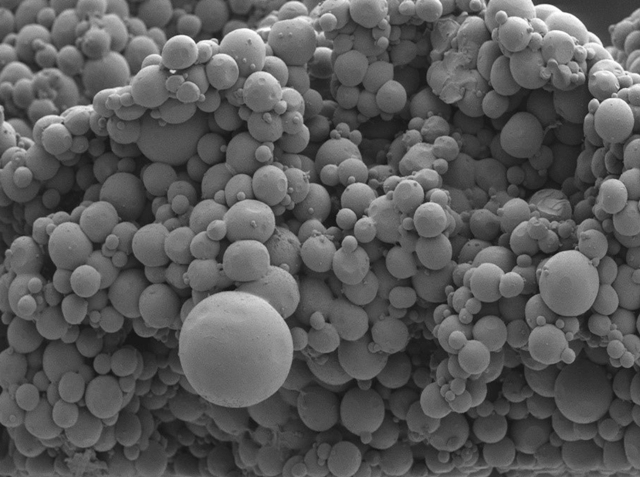
The team first uses an oil-and-water-emulsion to create tiny gels about 250 microns in diameter — 1 micron equals 1 millionth of a meter — then links the microgels together with microbial transglutaminase. The result is a bulk hydrogel with large enough pores to allow cells to flow through, yet also exhibits the same physical properties as non-porous hydrogels. In lab tests, the porous hydrogel allows human skin cells to transfer through the material, while earlier non-porous hydrogels block the skin cells.
Further tests show the porous hydrogel can also carry proteins that encourage wound healing. The researchers added platelet-derived growth factors, proteins that regulate cell growth and proliferation, to the hydrogel and show that the hydrogel can control the release of these proteins to boost the wound-healing capabilities of the hydrogel.
In addition, the team injected the hydrogel in the corneas of eyes excised from pigs, where the hydrogel adhered to the tissue for 2 weeks. Tests show during that time large numbers of cornea cells migrated into the pores of the hydrogel, indicating its potential as an treatment for eye injuries.
More from Science & Enterprise:
- Bio-Friendly Film Material Devised from Silk, Carbon Nanotubes
- Licensing Deal for Bioinks in 3-D Printed Transplant Lungs
- Protein Delivered with Gold Nanoparticles Helps Fix Muscle Injuries
- Nanoscale Sponges Deliver Rheumatoid Arthritis Treatment
- RNA Nanoparticles Designed for Brain Cancer Therapy
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.