16 Nov. 2020. Researchers devised a technique that in lab mice carries immune system enzymes on red blood cells to stop the spread of cancer in the lungs. A team from the Wyss Institute for Biologically Inspired Engineering at Harvard University describes the technique in today’s issue of the journal Nature Biomedical Engineering (paid subscription required).
Metastatic tumors are those that spread from the original tumor to other parts of the body, particularly the lungs. And metastatic tumors, say the authors, often are shielded from immunotherapies, treatments invoking the immune system, by tumors’ microenvironment, a matrix of blood vessels, normal cells, and extracellular matrix that supports tumor growth. Metastatic tumors can also be deeply embedded in the lungs, making them even more difficult to treat.
Researchers from the biomedical engineering lab of Samir Mitragotri are seeking ways of treating these difficult metastatic lung tumors and are taking an approach far different from conventional cancer immunotherapies. Instead of attacking the primary tumor, Mitragotri and colleagues focus first on stopping the spread of cancer to the lungs.
“Our approach is the exact opposite of conventional cancer treatments that focus on getting the immune system to recognize and attack the primary tumor,” says postdoctoral scholar and co-first author Zongmin Zhao in a Wyss Institute statement, “because those tumors are often large and difficult for immune cells to penetrate. We recognized that the high density of blood vessels in the lungs provides much better access to tumors there, offering a unique opportunity to induce an immune response by targeting the metastasis.”
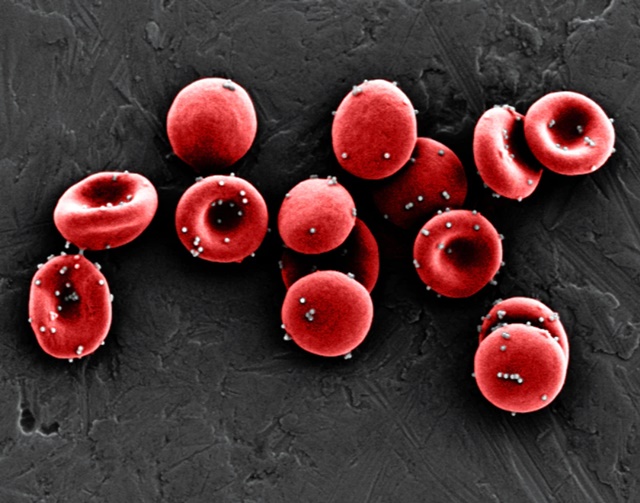
Mitragotri’s lab studies drug delivery technologies, including red blood cells as a delivery vehicles for nanoscale particles with therapeutic cargoes. In this case, the team developed nanoparticles filled with an immune-system enzyme that attach to red blood cells. The enzyme, known as CXCL10, stimulates responses from natural killer cells and T-cells in the immune system. The nanoparticles are made of poly lactic-co-glycolic acid or PLGA, a widely used biocompatible and biodegradable polymer, and coated with ICAM1, a cell surface protein to bind with blood vessel cells in the lungs.
The particles are designed to carry CXCL10 through the blood stream on red blood cells, deep into the metastatic lung tumors, where they release their cargoes. The researchers tested their drug delivery method on lab mice induced with metastatic lung cancer. The results show the drug-laden nanoparticles delivered on red blood cells stay in the mice lungs for up to six hours, largely accumulating in or near the metastatic tumors and expressing CXCL10 for up to 72 hours. Testing lung cells after injection of nanoparticles shows more T-cells and natural killer cells from the immune system to help and attack cancer cells, than before the injections.
Further tests show the mice receiving CXCL10 nanoparticles have fewer metastatic tumor modules than mice receiving direct injections of CXCL10 or empty nanoparticles alone. And mice receiving CXCL10 nanoparticles also have longer survival times — in a quarter of the cases, twice as long — than mice getting CXCL10 or empty nanoparticles alone. In addition, mice receiving the CXCL10 nanoparticles develop memory T-cells, which appear to protect against a return of the same tumor type and severity, when challenged later with lung cancer cells.
Harvard University filed for a patent on the technology with Mitragotri, Zhao, and co-first author Anvay Ukidve, now with Sanofi, as inventors.
More from Science & Enterprise:
- Personal Cancer Vaccine Induces Tumor Shrinkage
- Precision Drug Trial Shows Solid Tumor Shrinkage
- Start-Up Developing Engineered B-Cell Therapies
- Cancer Center, Biotech Partner on Off-the-Shelf T-Cells
- New Company IDs Drugs Targeting Cancer Cell Networks
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.