26 April 2016. A pharmaceutical company in Sweden is collaborating with University of Pennsylvania’s medical school in preclinical studies of a new drug that protects against long term damage caused by traumatic brain injury. Financial terms of the agreement between NeuroVive Pharmaceutical AB in Lund, Sweden and the university were not disclosed.
NeuroVive develops drugs based on cyclosporine, a common compound used largely to suppress the immune system for preventing rejection in organ transplants. The company’s work extends another property of cyclosporine, to protect mitochondria in nerve cells following traumatic injuries. Mitochondria are components in cells that provide energy for the cells at large.
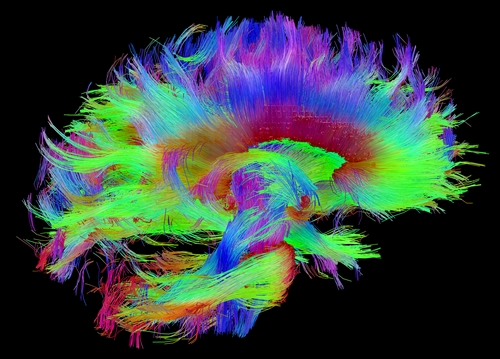
Traumatic brain injuries are caused by a blow to the head or penetrating head wound, such as a gun shot, that disrupt the normal functioning of the brain. The effects can be minor and temporary, such as concussions, but some can cause extended loss of consciousness. Centers for Disease Control and Prevention say 138 people in the U.S. die every day from traumatic brain injuries, accounting for 30 percent of all injury deaths.
One of NeuroVive’s lead products is NeuroStat, for protecting nerve cells in the brain from deterioration following traumatic brain injury. The drug is designed to prevent the deterioration of brain cells beyond the immediate injury caused by biochemical reactions, including calcium overload, inflammation, and oxidative damage. NeurStat is given as an infusion after patients with severe head injuries are stabilized.
While NeuroStat is undergoing an intermediate-stage clinical trial with traumatic brain injury or TBI patients, the company is engaging Penn’s medical school to test additional treatment options for the drug. Professor of bioengineering Susan Margulies and Todd Kilbaugh, a professor of anesthesiology and critical care, will lead the preclinical studies. Findings from the preclinical studies are expected to support the company’s regulatory submissions.
“We have been working for several years to develop clinically relevant experimental models of TBI,” says Margulies in a NeuroVive statement, “and believe that the testing of novel pharmaceutical treatments in our models, such as NeuroStat, will facilitate and improve the future clinical development of TBI.”
Read more:
- Stent Implants Demonstrated to Transmit Brain Activity
- Biodegradable Brain Sensors Developed, Tested
- Detailed Brain Activity Imaging Being Developed
- Biotech to Explore Gut-Brain Connections, Raises $44M
- Advocacy Group, Genetics Company Partner on Brain Disorder
* * *

 RSS - Posts
RSS - Posts
The second stage of damage to the brain takes place after the initial insult, as the injury continues to develop and worsen in the hours and days following the initial trauma. In this secondary stage, the trauma to the brain triggers a series of cascading intra-cellular biochemical reactions that end up causing severe demise of brain cells, brain damage and expanded disability. If this secondary stage can be mitigated, the eventual damage and disability can be greatly reduced, enabling the victim to get closer to full recovery.