24 January 2018. A bioengineering lab is receiving a National Institutes of Health grant to advance development of more tolerable synthetic veins and arteries implanted in heart bypass patients. The National Heart, Lung, and Blood Institute awarded more than $672,000 for the 1-year project to a team at University of Pittsburgh, led by bioengineering professor Jonathan Vande Geest.
Vande Geest’s Soft Tissue Biomechanics Lab studies new materials to improve the performance of soft tissues in the body, or create safe replacement tissue, including blood vessels. Replacement blood vessels are a critical need in coronary artery bypass surgery, where the first choice for surgeons is grafting the patient’s own veins or arteries from the leg or the mammary artery below the rib cage. But when the patient’s condition makes those options unavailable, synthetic blood vessel grafts are needed.
Synthetic grafts replacing large-diameter blood vessels usually work well for heart surgery patients, lasting up to 10 years. With small-diameter replacement vessels, however, problems often develop with immune-system reactions to the implants, causing the vessels to become clogged or form blood clots. “Small-diameter vascular grafts, or grafts involving blood vessels with an internal diameter smaller than five millimeters,” says Vande Geest in a university statement, “have much higher failure rates than larger ones. A significant proportion of vascular disease cases involve small-diameter blood vessels, so the demand for viable treatment options is very high.”
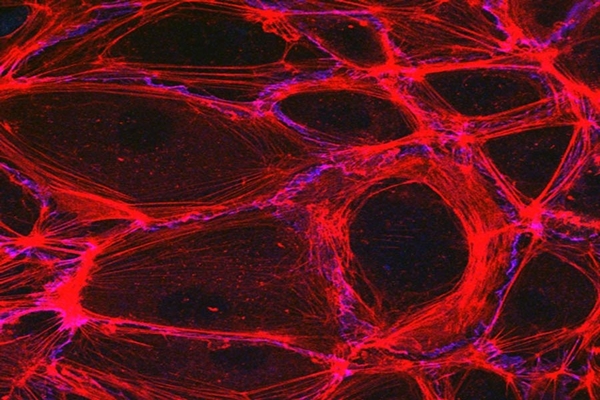
The Pittsburgh team proposes developing replacement grafts that more closely emulate natural blood vessels, to limit or eliminate these immune reactions. The researchers are building their replacement vessels with alternating layers of biomaterials gelatin and tropoelastin to replace the collagen and elastin respectively in natural blood vessels. Gelatin is derived from collagen, while tropelastin is a precursor material for elastin. The synthetic vessels will likewise be lined with endothelium, the natural lining of blood vessels, drawn in this case from blood.
The project calls for Vande Geest and colleagues to produce prototype synthetic vascular grafts for testing in small and large lab animals, rats and sheep, to verify their functional and mechanical properties. The tests include trials with endothelium cells in the lining of grafts from adult sheep as well as umbilical cord blood. The goal is a blood vessel graft, ready for clinical trials, compatible with a recipient’s immune system, and does not result in vascular disease from closure or blood clots.
“We believe our method of mimicking native artery microstructure and mechanics will result in a successful tissue-engineered graft,” notes Vande Geest, “and this grant will support trials to perfect both our experimental and computational approach.”
More from Science & Enterprise:
- Stem Cell Patches Shown to Treat Heart Attack Damage
- RNA Injections Shown to Rebuild Damaged Heart Muscle
- NIH Funds Heart Tissue Regeneration Tests in Pigs
- Injectable Patch Designed to Repair Heart Tissue
- Synthetic Beating Heart Repair Tissue Being Developed
* * *

 RSS - Posts
RSS - Posts
You must be logged in to post a comment.