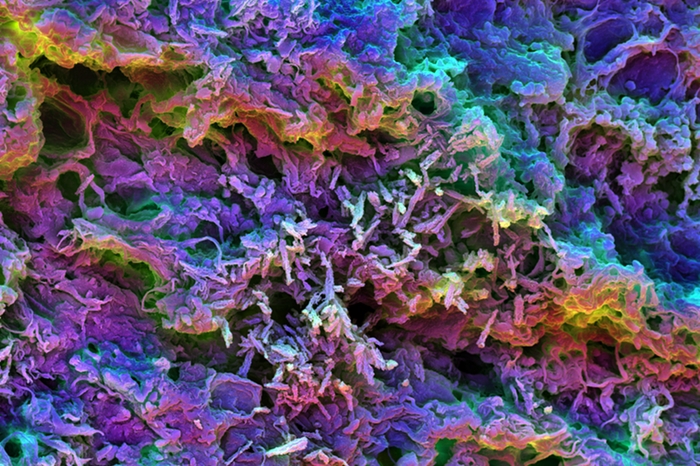
Scanning electron micrograph of scaffolds made of silica rods and PEI polymer (Wyss Institute, Harvard University)
5 March 2018. A Harvard University bioengineering lab developed an injectable material designed to load up with proteins from a patient’s own tumors to induce immune reactions that fight that person’s cancer. Findings from tests with lab mice conducted by a team from Harvard’s Wyss Institute appear in today’s issue of the journal Nature Materials (paid subscription required).
Researchers from the lab of Wyss Institute professor David Mooney are seeking ways to improve the performance of a promising and emerging form of cancer immunotherapy, known as neoantigens, unique sets of mutations expressed in cancer patients’ tumors. Neoantigens are peptides, short chains of amino acids resembling proteins, expressed by cancer patients’ tumors. In sufficient quantities and durability, neoantigens can provoke immune responses from T-cells, white blood cells in the immune system that fight disease-causing invaders, including cancer cells.
Neoantigens, however, are not very stable in the body, and can be broken down and cleared quickly. As a result, say the authors, many treatments based on neoantigens up to now require modifying the peptides, which detract from their effectiveness. The optimum solution, therefore, is one that delivers neoantigens in their original form, but still in large enough quantities and protected from degradation.
The Wyss Institute team — with associates from Dana-Farber Cancer Institute affiliated with Harvard, and institutions in Korea — applied their earlier work on biomaterials for cancer immunotherapy injections. As reported in Science and Enterprise, Mooney and colleagues devised a technique that injects porous silica rods that accumulate under the skin to form three-dimensional scaffolds, in which antigens that provoke an immune response can be placed. Mooney’s lab later developed an injectable water-polymer hydrogel that also provides a framework for delivering antigens.
In the new study, the team led by first author and graduate student Aileen Li, now a postdoctoral researcher at University of California in San Francisco, returned to the porous silica rods, but this time filled with the polyethyleneimine, or PEI, a biocompatible polymer. PEI is able to transport genes into cells, and thus is a candidate for carrying neoantigen peptides into dendritic cells, or DCs, in the lymph nodes that serve up antigens for disease-fighting T-cells.
Li says in a Wyss Institute statement that adding PEI into the silica rods, “enabled ready absorption of multiple peptides regardless of their inherent properties without the need to further modify them. And by being taken up by DCs together with the peptides, PEI enhanced the stimulation of DCs and the ensuing tumor-directed cytotoxic T cell responses in our mouse models.”
The mice in one set of tests were induced with cervical cancer from human papillomavirus, or HPV. Using a vaccine with silica rods and PEI polymers laden with an E7 peptide associated with HPV cancers, the large established tumors were eradicated from about 80 percent of the mice and extended their survival by 150 days. In addition, the vaccines invoked a durable protection against further HPV-associated tumors for 6 months.
Another series of tests induced mice with cancers that spread to the lungs, in which the silica-PEI vaccine scaffolds were filled with peptides derived from melanoma and colon cancer. The results show the metastatic lung tumors were eradicated in mice receiving these vaccines, as well as provoking strong immune reactions against the primary melanoma and colon cancers. Still other tests show the silica-PEI vaccine boosted the performance of checkpoint-inhibitor immunotherapies that remove the checkpoints or barriers to the immune system acting against cancer cells.
“Our materials approach,” adds Mooney, “is able to mix and match predicted neoantigens very easily and efficiently in a single scaffold that as a delivery vehicle could be plugged into existing pipelines to enable more effective personalized cancer treatments.”
More from Science and Enterprise:
- Biotechs Collaborate on Immunotherapies in $1.2B Deal
- Report: 19 New Precision Medicines Approved in 2017
- Biotechs Partner on HPV Cancer Immunotherapies
- Trial Underway Testing Personal RNA Cancer Drug
- Zymeworks, Janssen in $1.45B Antibody Licensing Deal
* * *

 RSS - Posts
RSS - Posts
[…] 3-D Biomaterial Boosts Personal Cancer Immunotherapy […]