8 March 2018. A team at Rice University in Houston developed an injectable gel material that in lab mice slows the release of cancer immunotherapy drugs, enhancing the treatments’ effectiveness and reducing the need for repeated doses. Researchers led by Rice University chemistry and bioengineering professor Jeffrey Hartgerink describe the material in the May 2018 issue of the journal Biomaterials (paid subscription required).
The Rice team is addressing a problem with stability and staying power of some cancer immunotherapies, treatments that invoke the immune system to attack cancer cells. A class of cancer immunotherapies called stimulator of interferon genes or Sting, agonists are showing promise in counteracting the ability of tumors to suppress the immune system, with some of these treatments now reaching clinical trials. Sting agonists on their own, however, break down and are cleared quickly by the body after injection, and as a result, require multiple injections. This instability, say the authors, also decreases the effectiveness of Sting agonists with more aggressive tumors.
Hartgerink and colleagues study hydrogels, water and polymer gel substances that mix with peptides, short chains of amino acids resembling simple proteins. Among the lab’s projects are multi-domain peptide hydrogels that resemble the framework structure of cells and provide an environment that encourages cell and tissue growth. Hydrogels can also be liquefied, making them injectable with a ordinary syringe directly to a tumor site, then return to their gel-like state after injection.
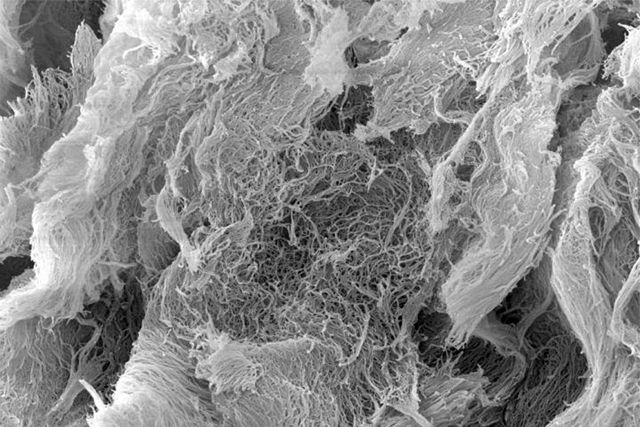
In this project, the researchers developed a peptide hydrogel they call StinGel to deliver Sting agonist cancer treatments. The hydrogel base of StinGel is positively charged and reassembles into a 3-D gel with a nanofiber matrix after injection. The team tested StinGel first in lab cultures, then in 6 groups of 10 mice, implanted with head and neck cancer cells, against Sting agonist drugs alone, and mixed with ordinary collagen hydrogels for comparison.
The results show the StinGel released Sting agonists over an extended period 8 times longer than the collagen hydrogel. In addition, 6 of the 10 the mice injected with StinGel survived for 105 days after their treatments, compared to 1 in 10 mice receiving the Sting agonists alone or with collagen hydrogel. And the StinGel-recipient mice developed a resistance to later cancer cell implants, suggesting the treatments induced an immunity to future occurrences of the cancer.
The authors conclude StinGel offers a feasible delivery method for Sting agonists, also known as cyclic dinucleotides, or CDNs. StinGel, says Hartgerink in a university statement, “provides a unique environment for the release of CDN that other gels just can’t match.” He adds, “We think that our StinGel approach has the potential to significantly broaden the scope of this powerful immunotherapy drug to a larger range of resistant cancers.”
More from Science and Enterprise:
- 3-D Biomaterial Boosts Personal Cancer Immunotherapy
- Biotechs Collaborate on Immunotherapies in $1.2B Deal
- Biotechs Partner on HPV Cancer Immunotherapies
- Alliance Exploring Microbiome on Cancer Immunotherapy
- Zymeworks, Janssen in $1.45B Antibody Licensing Deal
* * *

 RSS - Posts
RSS - Posts
[…] Peptide Hydrogel Boosts Cancer Immunotherapies […]