Researchers at Brown University in Providence and Harvard Medical School in Boston have created a three-dimensional living tissue model of the brain, including surrounding blood vessels, to study potential brain tumor treatments. The team of chemistry and biomedical engineering researchers published their findings in the journal Theranostics.
The need for a living tissue model arose from the shortcomings of tests using petri dishes that failed to adequately model the behavior of some brain cells when interacting with tumors. Chemistry graduate student Don Ho, the first author of the Theranostics paper, created the tissue model with hydrogel made of agar.
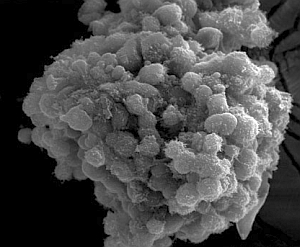
Ho and his colleagues introduced to the model a glioma or brain tumor from a rat, which the team used for its research. The researchers added to the model endothelial cells that line cow respiratory blood vessels, and which congregated around the tumor to create the blood vessel architecture that feed the tumor oxygen and nutrients.
The three-dimensional tissue model enabled the researchers to observe the interaction of the endothelial cells with the tumor, which the petri dish tests did not allow. In petri dishes, the endothelial cells separated from, rather than attached to, the substrate. This property of the tissue model let the team study tumor formation and growth, as well as the actions of test treatments, in an environment more like that of a living organism.
In their experiments, the Brown/Harvard team tested iron-oxide nanoparticles with the chemical tumstatin added to penetrate the blood vessels that sustain the tumor. Iron-oxide nanoparticles are useful for diagnostics, since they can bind to endothelial cells and be tracked by magnetic resonance imaging. The researchers knew from previous studies that tumstatin was effective at blocking endothelial cell growth in gliomas.
The research team then attached tumstatin, a naturally occurring protein found in collagen, to iron-oxide nanoparticles and dosed the model. As expected, the nanoparticles were taken in by the endothelial cells. In a series of subsequent experiments, the team reported the tumstatin/iron-oxide nanoparticles decreased blood vessel growth 2.7 times more than under normal conditions, over eight days.
The 3-D model allowed the glioma and the endothelial cells to assemble naturally, say the researchers, just as they would in real life. Using the living 3-D model, the tests by the Brown/Harvard researchers confirmed the ability of iron-oxide nanoparticles to reach blood vessels surrounding a glioma as well as the ability of tumstatin to penetrate endothelial cells.
“You want to see nanoparticles that diffuse through the endothelial cells, says Ho, “which is lost in 2-D because you just have diffusion into media.”
Read more:
* * *

 RSS - Posts
RSS - Posts
[…] Read more: Living Tissue Cell Model Developed to Study Brain Tumors […]